
Tobacco-use prevention and public awareness in the DRC
While global awareness of tobacco-related harms continues to grow, less attention has been given to the upstream factors sustaining tobacco use. In the Democratic Republic of the Congo (DRC), these factors include widespread tobacco farming, regulatory gaps, and persistent exposure to commercial influences, especially in vulnerable rural communities.
In line with Article 12 of the World Health Organization Framework Convention on Tobacco Control (WHO FCTC), which underscores the role of education, communication, training, and public awareness in tobacco control, this page shifts the focus from reactive health responses to proactive prevention, beginning with root-cause interventions.
It introduces a four-part framework, from pre-primary to tertiary prevention, grounded in strategic actions proven effective in other country contexts. Drawing on global best practices and empirical evidence, this page highlights actionable pathways for the DRC to reduce tobacco and nicotine use and exposure across the population, starting well before initiation.

Pre-primary tobacco prevention refers to upstream strategies that seek to address the root causes and enabling environments that lead to tobacco and nicotine product use before individuals are ever exposed. Rather than focusing solely on individual behavior, these strategies intervene at the social, environmental, and commercial levels, disrupting the systems that normalize and promote tobacco and nicotine consumption.
This level of prevention is crucial in low- and middle-income countries (LMICs) like the DRC, where aggressive tobacco industry tactics, limited regulatory enforcement, and socio-economic vulnerabilities converge to increase population-level risk, particularly among youth and rural communities.
To prevent tobacco use in the DRC, strategies must address root causes: economic reliance on tobacco, weak regulations, and industry interference, especially as a youthful population of 112.8 million (by 2025) faces high initiation risks.DRC Population (1950-2025)
Source: Worldometer
The tobacco industry in many LMICs, including the DRC, continues to deploy well-established tactics to attract youth, such as distributing free samples, sponsoring community events, and marketing flavored products tailored to first-time users.
Despite ratifying the WHO FCTC in 2005 and the minister order n°1250/CAB/ MIN/SPHP/ 041/DCA/PNCLT/2022, tobacco brands are still visible near schools, in public markets, and in local media. This regulatory gap allows the tobacco industry to shape favorable public perceptions and normalize tobacco use in daily lives.Key strategies for pre-primary prevention: Global insights
The following global insights illustrate how upstream measures have been effectively employed to reduce tobacco use across diverse contexts.
- Promoting alternative crops to replace tobacco
- Advertising and sponsorship bans
- Taxation and price controls to deter youth initiation
- Smoke-free laws in public places
- Community mobilization and advocacy
Promoting alternative crops to replace tobacco
Although tobacco farming still exists in the DRC, with 3,479 tons produced in 2020 despite occupying just 0.03% of agricultural land. This reflects limited livelihood options for farmers in affected areas.
Global evidence shows that supporting farmers to transition to alternative crops reduces dependence on tobacco and strengthens rural resilience.In Kenya, programs supporting crops like sweet potatoes and legumes improved income stability.
India’s crop substitution in Andhra Pradesh showed higher profitability from chillies and groundnuts. In Malawi, soybeans and paprika proved viable alternatives, especially when supported by cooperatives and buyer contracts.Recommendation:
The DRC should implement a national program to diversify crops and help tobacco farmers transition to more sustainable and profitable alternatives, drawing on global best practice. The program should include:
- Training in alternative crop production and agribusiness skills.
- Access to inputs and shared equipment to support new farming activities.
- Cold storage facilities to reduce post-harvest losses.
- Support for cooperative marketing and buyer contracts.
- Policy incentives to reduce reliance on tobacco and promote long-term rural resilience.
This approach would reduce dependence on tobacco farming, improve farmer incomes, and align with national public health priorities.
Advertising and sponsorship bans
The WHO FCTC Article 13 provides the legal foundation for a comprehensive ban on all forms of tobacco advertising, promotion, and sponsorship (TAPS).
Evidence shows that full bans are far more effective than partial ones, which leave exploitable gaps. In the DRC, legal provisions prohibiting tobacco advertising and sponsorship have been in place since 2007. Ministerial Decree No. 008/CAB/MIN.INFO.PRES & COM.NAT./2007 sets the criteria for advertising tobacco and alcoholic beverages, and the more recent Ministerial Order No. 1250/CAB/MIN/SPHP/ 041/DCA/PNCLT/2022 prohibits the advertising, promotion, and sponsorship of tobacco, tobacco products, and their derivatives, as well as smoking in public places. These provisions are essentially based on partial bans and do not yet fully comply with the major recommendations of the guidelines in Article 13 of the FCTC.Internationally, Uganda’s 2015 Tobacco Control Act exemplifies a strong TAPS ban, helping reduce public exposure despite enforcement challenges.
Canada’s 2016–2017 report highlights federal monitoring and enforcement, contributing to lower youth exposure. Turkey paired its TAPS ban with plain packaging, leading to reduced tobacco use. In the Philippines, Joint Memorandum Circular 2010-01 reinforced policy independence by limiting government interaction with the tobacco industry and requiring transparency.Recommendations to strengthen TAPS implementation:
- Implement Ministerial Order No. 1250/CAB/MIN/SPHP/041/DCA/PNCLT/2022.
- Review and strengthen Ministerial Decree No. 008/CAB/MIN.INFO.PRES & COM.NAT./2007.
- Establish independent monitoring and enforcement bodies to ensure impartial oversight of TAPS compliance.
- Conduct regular compliance audits to proactively identify and address violations.
- Imposing meaningful penalties for non-compliance will deter tobacco industry interference.
- Incorporate complementary measures, such as plain packaging and transparency rules, in government interactions with the tobacco industry.
- Integrate TAPS enforcement into existing health inspection systems to optimize resources and expand reach.
Taxation and price controls to deter youth initiation
Tobacco taxation is a proven, cost-effective strategy, especially effective among youth and low-income groups.
Countries like South Africa, the Philippines, and Mexico saw sharp declines in smoking following tax hikes. WHO estimates that a 10% price increase can cut tobacco use by up to 8% in LMICs, highlighting the power of fiscal policy in reducing consumption.In the DRC, the TaxSiM model provides a country-specific simulation tool to guide evidence-based tobacco tax policy.
By evaluating the fiscal and health impacts of different tax scenarios, including effects on new tobacco products, it helps policymakers craft taxation strategies that support both public health and sustainable revenue generation, reinforcing taxation as a vital pillar of global pre-primary prevention efforts.Smoke-free laws in public places
Comprehensive smoke-free laws protect non-smokers and help shift social norms around tobacco use. Countries like Brazil and Ireland saw health improvements and reduced smoking after such laws were enacted.
In the DRC, enforcement is limited, but expanding smoke-free zones, especially in schools, hospitals, and public transport, could play a key role in changing behavior and reducing exposure.Community mobilization and advocacy
Community-based strategies, particularly when supported by trusted leaders and institutions, are crucial in shaping local norms around tobacco use. A study emphasized that community engagement improves the reach and effectiveness of public health campaigns.
Examples of such community engagement include tobacco-free village pledges led by local authorities and partnerships with religious groups that deliver anti-tobacco messages during sermons, youth groups, or public gatherings.1. Case Insight:
In Senegal, Malicounda Bambara ended female genital cutting through community dialogue, led by Imam Demba Diawara.
This change was locally driven and sustainable. This demonstrates the power of trusted leaders to effect change in harmful social norms.2. Relevance to tobacco control in the DRC
The DRC could adopt this approach by engaging with religious and traditional leaders. These figures hold significant influence and can promote smoke-free norms. Their involvement could reduce tobacco initiation, particularly among young people.
3. Communication channels
Combine community leadership with local radio and outreach tools.
Use culturally relevant messaging to engage rural and low-literacy groups. This low-cost approach ensures a wide reach and builds community trust.
Primary prevention refers to interventions designed to stop individuals from initiating tobacco use, with a particular focus on youth and other vulnerable populations. Unlike secondary or tertiary strategies, which address existing tobacco users, primary prevention operates before tobacco use begins, targeting awareness, attitudes, and decision-making at an early stage. The Institute for Work & Health (IWH) defines primary prevention as action taken to prevent the onset of disease or harmful behavior by reducing exposure to risk factors.
In the DRC, primary prevention efforts face critical challenges, including limited public awareness, weak policy enforcement, and aggressive marketing tactics by the tobacco industry. Youth exposure to tobacco advertising remains widespread, with over 40% of adolescents reporting seeing tobacco promotions near schools or in public spaces.
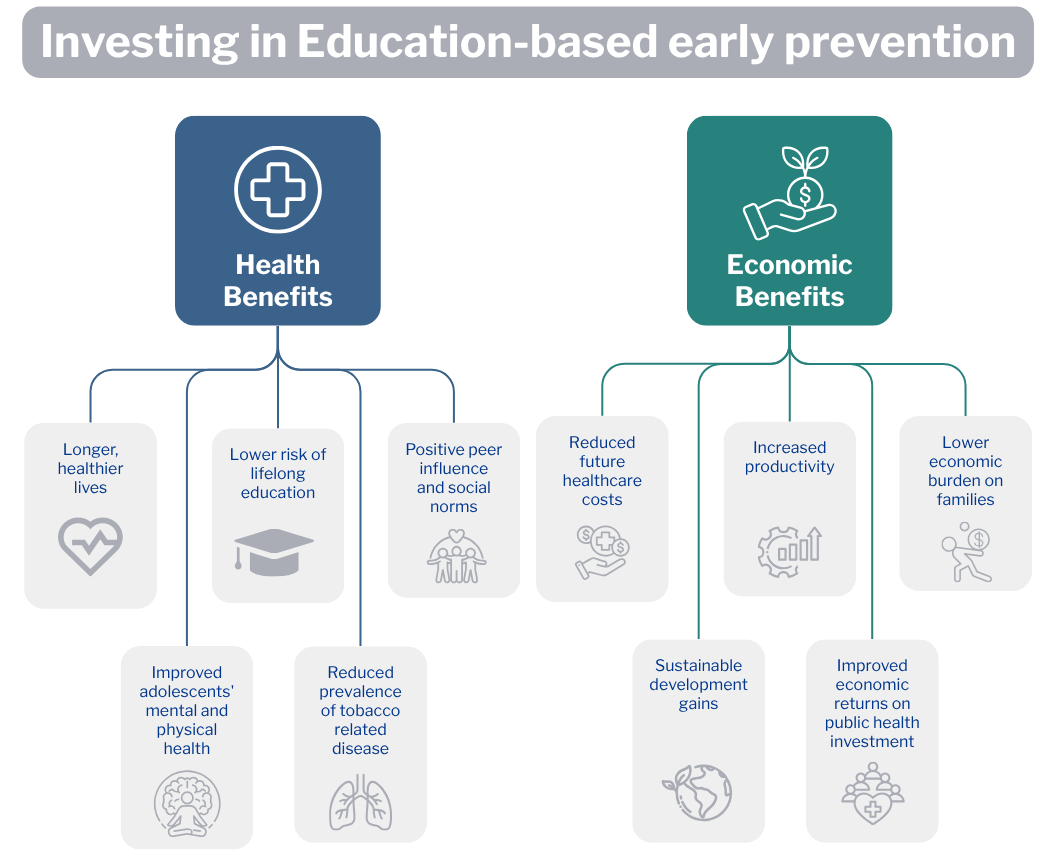
And most smokers begin before the age of 18, making early intervention essential.To fully understand the value of early tobacco prevention, it is important to consider not only the health outcomes but also the broader economic implications.
Tobacco use places a heavy burden on countries like the DRC, harming both public health and economic stability. While health impacts are widely documented, the economic impact is often overlooked. Investing in primary prevention is not only a public health imperative but also an economically sound strategy. The WHO FCTC has developed investment cases for different countries across the globe that analyze both the health and economic costs of tobacco use, as well as the potential economic benefits of implementing key prevention measures. These investment cases provide policymakers with country-level evidence to inform tobacco control policy-making.
Furthermore, a study analyzing 21 LMICs also found that implementing WHO FCTC demand-reduction and prevention strategies would provide a positive return on investment in every country analyzed. This means that the economic benefits, such as reduced healthcare costs and increased productivity, outweigh the costs of implementing these tobacco control policies.Early intervention, particularly before the age of 18, is crucial to primary prevention. According to the United Nations Development Programme (UNDP), ministries of education can play a significant role in enforcing tobacco-free schools and integrating prevention into curricula. Evidence from a Cochrane review of over 140,000 students shows that school-based programs, especially those building peer resistance, effectively reduce smoking uptake.
In Indonesia, a program targeting 12–13-year-old boys led to a 6.5% increase in abstinence and strong economic returns.Similarly, enforcement of smoke-free school policies across 43 countries correlates with lower youth smoking, and Iceland’s national “Drug-Free Iceland” strategy, implemented in schools between 1997 and 2002, significantly reduced youth smoking rates with a lasting impact.
In the DRC, where youth make up a large share of the population, school-based prevention should be a national priority for long-term tobacco control.
These findings reinforce the need for countries like the DRC to adopt structured, evidence-informed interventions that prevent tobacco uptake before it begins.
Key strategies for primary prevention: Global insights
To be effective, primary prevention must be both contextually relevant and grounded in global best practices. The following approaches have shown success in various settings and offer adaptable models for the DRC to adopt.
- Health education campaigns targeting youth
- School- and curriculum -based tobacco prevention programs
- Family-based behavior interventions
- Mobile and digital interventions for adolescents
- Restrictions on sales to minors
Health education campaigns targeting youth
Mass media and peer-driven campaigns have proven effective in reshaping youth perceptions of tobacco use. A recent systematic review and meta-analysis of 476 studies found that anti-tobacco campaigns, smoking bans, health warnings, and tax increases are among the most effective population-level policies for reducing smoking behavior, with consistent evidence showing their positive impact on cessation rates, smoking prevalence, and tobacco sales.
Campaigns are most successful when they use youth-centered narratives, local languages, and participatory content development.School- and curriculum-based tobacco prevention programs
Schools represent a strategic entry point for primary prevention, offering consistent opportunities to influence youth attitudes toward tobacco use.
Integrating tobacco prevention into classroom curricula, particularly using interactive modules focused on life skills, peer pressure resistance, and critical thinking, has led to significant reductions in smoking initiation in countries like Finland and India. These programs are most impactful when supported by national education policies and delivered by trained educators.Family-based behavior interventions
Parental involvement enhances the effectiveness of youth-focused interventions. Programs such as “Family Matters” in the U.S. have shown that structured conversations between caregivers and adolescents about tobacco use can strengthen refusal skills and reduce experimentation.
In settings where tobacco use is normalized in the household, family-based approaches or family therapy also serve to interrupt intergenerational cycles of use.Mobile and digital interventions for adolescents
With mobile phone access expanding in many LMICs, digital tools have emerged as scalable and cost-effective prevention methods. In India and South Africa, SMS campaigns and interactive mobile apps have been piloted to deliver age-appropriate content, motivational messaging, and behavioral nudges to reduce tobacco initiation.
These tools can be customized for local dialects, cultural references, and digital literacy levels.In the DRC, existing mobile health platforms, such as m-Jang and U-Report, have been used to promote maternal health, youth engagement, and disease prevention.
These platforms could be adapted to include tobacco prevention messaging targeted at adolescents, particularly in regions with high mobile penetration. Aligning tobacco content with broader youth health initiatives may enhance uptake and sustainability.Restrictions on sales to minors
Legal prohibitions on tobacco sales to individuals under 18 are central to primary prevention. However, in the absence of active enforcement, such laws are often ineffective. In Brazil and Turkey, combining legislation with regular vendor compliance checks and penalties has led to significant reductions in illegal sales to minors.
The DRC can learn from these experiences by strengthening licensing systems, training vendors, and involving communities in monitoring and enforcement. To reinforce these efforts, family-based programs and community sensitization can address the normalization of tobacco use at home. Promoting smoke-free households and caregiver awareness supports broader prevention goals.Collectively, these interventions offer a roadmap for implementing comprehensive primary prevention in the DRC. When combined with upstream policy actions, they can establish protective environments that delay or prevent tobacco initiation and reduce long-term public health burdens.
Secondary prevention focuses on identifying and supporting individuals who regularly use tobacco and nicotine products but have not yet developed long-term dependency or disease. This stage is crucial for reducing the progression of use and preventing chronic health consequences. The Institute for Work & Health (IWH) defines secondary prevention as early intervention aimed at detecting and addressing risk behavior in its initial stages to halt further harm.
Tobacco and nicotine use in the DRC remains a pressing concern, with multiple national surveys including the Global Youth Tobacco Survey (GYTS) 2008,
the Demographic and Health Survey (DHS) 2014, the Multiple Indicator Cluster Survey (MICS) 2017–2018, and the Data on Youth and Tobacco in Africa (DaYTA) Survey 2024, providing important insights into usage patterns and exposure. To explore detailed findings and monitor trends, please visit the TCDI DRC Prevalence page here.Key strategies for secondary prevention: Global insights
- Brief interventions by healthcare providers
- Quitline services and mobile cessation tools
- Pharmacotherapy for early-stage users
- Screening and counseling during clinical encounters
- Mass media cessation campaigns
Brief interventions by healthcare providers
Brief conversations during routine healthcare visits can significantly increase quit attempts, especially when delivered with empathy and followed by support. The United Kingdom’s “Very Brief Advice” (VBA) model, “Ask, Advise, Act,” has shown impact in under five minutes.
A similar approach could be adapted in the DRC’s primary care settings, particularly in maternal and outpatient services.An alternative model that could also be adopted is the 5As framework, which provides a simple, structured guide for tobacco cessation in DRC:
The 5As for tobacco and nicotine cessation:
- Ask about tobacco use.
- Advise on the benefits of quitting and the risks of continued use.
- Assess readiness to quit.
- Assist with resources, counseling, or medications.
- Arrange follow-up and continued support.
Note: Messaging should be adapted based on age, gender, and cultural context to increase effectiveness.
Quitline services and mobile cessation tools
Quitlines and mobile tools are effective, scalable solutions for helping people quit tobacco, especially in low-resource settings where in-person support is limited. These tools offer counseling, motivation, and quitting tips through phone calls, SMS, or apps.
- South Africa’s National Quitline, run by the National Council Against Smoking, provides free phone counseling and SMS support. It reaches both urban and rural users and has shown success in boosting quit attempts.
- India’s mCessation program delivers motivational SMS messages in multiple languages, reaching over 2 million users. It’s linked to the national quitline and helps users track progress and manage cravings.
- The U.S. Centers for Disease Control and Prevention’s quitSTART app supports young users through gamified behavior tracking, reminders, and custom quit plans.
- Canada’s Smokers’ Helpline and QuitNow BC combine live quitline services with SMS coaching and online chat.
While the DRC does not yet have national quitline services, similar programs could be adapted. A low-cost SMS model, linked with health clinics, could offer weekly messages, support, and local-language resources to help users quit. Partnering with faith-based clinics, which have wide reach in rural areas, could further expand access and trust, especially in underserved communities.
Pharmacotherapy for early-stage users
Nicotine Replacement Therapy (NRT) and medications like varenicline and bupropion are effective in reducing withdrawal symptoms and increasing quit success.
While access to pharmacotherapy is often limited in LMICs, pilot programs in countries like Jordan and Vietnam have shown that even small-scale NRT distribution can enhance cessation rates, especially when combined with counseling.The Congolese Ministry of Health could consider subsidizing NRT access and reducing detoxification costs, particularly for low-income users, to expand equitable support for those seeking to quit. It is also imperative to integrate tobacco control into the primary health care system in terms of minimum package of activities (MPA) and complementary package of activities (CPA) in health zones. The DRC has already developed an integrated approach to the prevention and treatment of substance abuse, including smoking, and strengthening this approach will be of great benefit to smokers who want to quit.
Screening and counseling during clinical encounters
Routine screening for tobacco use during maternal care, pediatric visits, and outpatient consultations creates opportunities to identify early users. In India’s mCessation program, screening integrated into antenatal care helped identify tobacco-exposed pregnant women, linking them to mobile-based cessation support.
This approach is especially relevant in the DRC, where maternal exposure and child secondhand smoke exposure are growing concerns.Mass media cessation campaigns
Public campaigns targeting current and occasional smokers can increase motivation to quit and direct users toward services. A systematic review on the effectiveness of graphic health warnings found that such warnings significantly increased perceptions of tobacco-related harm and intentions to quit, particularly when combined with emotionally resonant content such as testimonials.
Media-based cessation efforts are especially valuable in rural or low-literacy settings when delivered via radio or community broadcasts.To strengthen impact, graphic warnings on tobacco packaging should also be provided in local languages to reach rural smokers more effectively.
Tertiary prevention targets individuals already affected by tobacco-related illnesses, aiming to reduce complications, slow disease progression, and improve quality of life. This level of intervention is essential for minimizing the long-term health and economic burden associated with chronic diseases caused or worsened by tobacco use, such as cardiovascular disease, chronic obstructive pulmonary disease (COPD), and cancer. According to the Institute for Work & Health (IWH), tertiary prevention aims to reduce the long-term impact of ongoing illness or injury by helping individuals manage complex, chronic health conditions and improve quality of life.
In the DRC, tobacco-attributable illness and mortality remain a growing concern, but comprehensive data on the burden is still limited. To explore the latest available evidence on health impacts, please refer to the Tobacco Harm page for the DRC on the TCDI website here.Key strategies for tertiary prevention: Global insights
Tertiary prevention relies on several complementary interventions:
- Intensive behavioral therapy for heavy or long-term users
- Integration of cessation into non-communicable diseases (NCDs) care
- Smoking cessation support for hospitalized or chronically ill patients
- Palliative care for tobacco-related illness
Intensive behavioral therapy for heavy or long-term users
For long-term tobacco users, brief interventions may not be enough. Structured, multi-session behavioral therapy, delivered by trained counselors or psychologists, has shown significant success in countries like the United States and Germany.
These programs often include coping strategies, relapse prevention, and mental health integration. Such models could be adapted into urban referral hospitals in the DRC as part of NCD clinics.Integration of cessation into non-communicable diseases (NCDs) care
Countries like Thailand and Brazil have successfully embedded tobacco cessation into routine care for patients with NCDs.
For example, cardiology and oncology units routinely screen for tobacco use and offer counseling and pharmacotherapy. In the DRC, where NCD care is growing through specialized clinics, integrating cessation protocols into patient management pathways could improve recovery and reduce readmissions. To support implementation, task-shifting to nurses and community health workers is essential, ensuring consistent delivery of brief interventions even in resource-constrained settings.Smoking cessation support for hospitalized or chronically ill patients
Hospitalization offers a teachable moment for behavior change. Evidence from the UK and South Africa shows that providing cessation counseling and NRT during inpatient stays, especially for patients with smoking-related conditions, can significantly increase quit success and lower complication rates.
In the DRC, this approach could be piloted in provincial hospitals and tailored for conditions like stroke, tuberculosis, and respiratory infections.Tobacco cessation should be established as a standard component of hospital protocols to ensure consistent care and long-term health benefits.
Palliative care for tobacco-related illness
For patients with advanced tobacco-related diseases, palliative care focuses on pain management, psychological support, and dignity in end-of-life care. Rwanda’s national palliative care strategy offers a model for resource-limited contexts.
In the DRC, training frontline health workers in basic palliative skills and integrating these into community health structures could improve the quality of life for terminally ill tobacco users.National youth tobacco indicators for the DRC
Data Reliable and current national data are essential for assessing youth tobacco use and designing effective prevention strategies. While multiple surveys contribute to this landscape, national household surveys provide the most recent insights into tobacco-related behaviors among adolescents and youth in the DRC.These surveys capture key dimensions such as:
Disaggregated prevalence of tobacco and nicotine use, including data by product type, gender, age, urban/rural location, education level, socio-economic status, province, and self-reported reasons for tobacco useTo explore the full set of indicators and monitor trends, please refer to the Prevalence page for the DRC on the TCDI website here.
Proposed interactive scorecard
To support national planning and advocacy, we propose an interactive scorecard that evaluates progress in tobacco control across five key domains. Each domain is scored on a 0–3 scale (0 = no action, 1 = initial steps, 2 = moderate progress, 3 = strong implementation), with color coding to help visualize strengths and weaknesses. The colors correspond to scores: red = no action, yellow = initial steps, orange = moderate progress, green = strong implementation).
This scorecard can serve as a visual advocacy and planning tool. Ministries of Health and Education, civil society actors, and development partners can use it to identify priority areas for action and track progress over time. It can also be adapted into a digital dashboard for real-time updates and stakeholder engagement. To maximize its impact, capacity-building efforts should be directed at teachers and civil society organizations to ensure they can interpret and apply the scorecard effectively in their local contexts.
This module provides targeted information to key stakeholder groups responsible for shaping, financing, and implementing youth tobacco prevention strategies. It incorporates best practices, economic rationales, and practical steps toward stronger multisectoral action.
What ministries of education need to know
Model legislation: Ministries of Education should adopt policies that establish and enforce 100% tobacco-free schools. Model laws, such as those implemented in India and the Philippines, restrict tobacco sales within a designated distance from schools and ban sponsorships of school-related events.
Economic arguments: Education-based tobacco prevention generates long-term returns on investment as discussed earlier. According to WHO and UNDP, preventing youth initiation through school policies and curricula reduces tobacco-related health costs, increases lifetime productivity, and strengthens the human capital base.
Integration into national policies: Integrating tobacco education into national school curricula is both feasible and effective. Countries like Canada have embedded health education and smoke-free policies within their national strategy, yielding reduced adolescents smoking rates.
What Ministries of Health and Finance need to know
Cross-sectoral planning: Collaboration with the education sector is critical to ensure early and sustained intervention. Tobacco use often begins before age 18, and cost-effective prevention requires reaching adolescents early through health promotion in schools.
Economic benefits: Investment in prevention can yield a 12–20 times return in saved healthcare costs and increased productivity over time.
Earmarking a portion of tobacco tax revenue for public health education and cessation programs can strengthen and sustain these efforts.Data-driven policy: Monitoring and evaluation of school-based programs can guide national strategy and resource allocation. Available data from surveys provide useful insights; however, their coverage and frequency remain limited. Regular and expanded data collection, supported by tools like scorecards, is recommended to track progress and inform evidence-based policy-making. Scorecards and periodic data collection are recommended.
What civil society organizations (CSOs) and teachers need to know
School engagement: Teachers are frontline agents of change. When equipped with training and tools, they can deliver effective prevention messages and help create a culture of health in schools.
Community advocacy: Civil society actors can amplify prevention efforts by:
- Promoting smoke-free environments
- Monitoring advertising/sales to minors
- Supporting parental and teacher awareness and many other ways.
Local testimonials
Civil society in the DRC has long played a role in addressing tobacco and substance use, though its efforts were initially fragmented and lacked coordinated impact. Faced with a well-resourced and strategic tobacco industry, early advocacy by civil society often struggled to generate sustained influence.
Since 2014, however, a shift has occurred. A coalition of non-governmental organizations came together to form the ACCT (Alliance pour la Contrôle du Tabac), a platform dedicated to combating tobacco and drug addiction. This alliance has since become a pivotal actor in awareness-raising campaigns and policy engagement efforts.
Notably, ACCT contributed to the development and adoption of the 2018 framework law on public health, which incorporated key anti-tobacco measures, marking one of the first major legislative victories in tobacco control within Congolese law.ACCT continues to work in partnership with the Ministry of Health and the National Program for the Fight Against Drug Addiction and Toxic Substances, aiming to improve both medical and social care for individuals affected by addiction. This approach seeks to reduce the overall harm of tobacco use, especially among youth.
Testimonial Highlight: LSFT (Ligue pour la Santé des Fumeur et autre Toxicomane)
One notable example of grassroots engagement is the “Ligue pour la Santé des Fumeurs et autres Toxicomanes (LSFT)”, a non-governmental organization established in 2007 by a former smoker and drug user. Drawing from lived experience, the founder transformed personal recovery into a powerful advocacy tool by supporting former users through agro-pastoral entrepreneurship and peer outreach. Despite limited resources, LSFT remains active in raising awareness among youth about the harmful effects of tobacco and addiction, contributing to local-level behavior change.
These stories underscore the essential role of civil society in shaping tobacco control from the ground up, rooted in both community realities and institutional advocacy.
Recommendations:
- To amplify these efforts, testimonials should be collected in multiple local languages.
- Disseminate the content through national media campaigns to engage broader audiences and promote relatable, community-based narratives.
Conclusion
This page presents a forward-looking approach to tobacco prevention in the DRC, one that goes beyond treating symptoms and instead targets the root causes of tobacco use. Using a four-level prevention framework, it offers practical, scalable strategies to reduce exposure, delay youth initiation, and manage long-term health impacts, especially in low-resource settings.
The success of this approach depends on more than just the health sector. Ministries of Health, Education, and Finance must work together; sharing plans, budgets, and responsibilities, to create a strong, unified national response. To make lasting progress, the government must show strong leadership, commit to steady funding, and ensure that civil society, local communities, and development partners are fully engaged. Grounded in both local realities and global evidence, this framework lays the foundation for a healthier, tobacco-free future for the DRC.

